Glaucoma Exam Toowoomba | Glaucoma Exam Highfields
Glaucoma
Overview
Glaucoma is a group of eye conditions that damage the optic nerve, the health of which is vital for good vision. This damage is often caused by an abnormally high pressure in your eye.
Glaucoma is one of the leading causes of blindness for people over the age of 60. It can occur at any age but is more common in older adults.
Many forms of glaucoma have no symptoms. The effect is so gradual that you may not notice a change in vision until the condition is at an advanced stage.
Because vision loss due to glaucoma can’t be recovered, it’s important to have regular eye exams that include measurements of your eye pressure so a diagnosis can be made in its early stages and treated appropriately. If glaucoma is recognised early, vision loss can be slowed or prevented. If you have the condition, you may need treatment for the rest of your life.
Symptoms
The signs and symptoms (if any) of glaucoma vary depending on the type and stage of your condition. For example:
Open-angle glaucoma
- Patchy blind spots in your side (peripheral) or central vision, frequently in both eyes
- Tunnel vision in the advanced stages
Acute angle-closure glaucoma
- Severe headache
- Eye pain
- Nausea and vomiting
- Blurred vision
- Halos around lights
- Eye redness
If left untreated, glaucoma will eventually cause blindness. Even with treatment, about 15 percent of people with glaucoma become blind in at least one eye within 20 years.
When to see an optometrist:
Promptly go to an emergency room or an optometrist if you experience some of the symptoms of acute angle-closure glaucoma, such as severe headache, eye pain and blurred vision.
Causes
Glaucoma is the result of damage to the optic nerve. As this nerve gradually deteriorates, blind spots develop in your vision. For reasons that doctors don’t fully understand, this nerve damage is usually related to increased pressure in the eye.
Elevated eye pressure is due to a buildup of a fluid that flows throughout the inside of your eye. This internal fluid normally drains out through a tissue called the trabecular meshwork at the angle where the iris and cornea meet. When fluid is overproduced or the drainage system is compromised the fluid can’t flow out at its normal rate and eye pressure increases.
Glaucoma tends to run in families. In some people, scientists have identified genes related to high eye pressure and optic nerve damage.
Types of glaucoma include:
Open-angle glaucoma
Open-angle glaucoma is the most common form of the disease. The drainage angle formed by the cornea and iris remains open, but the trabecular meshwork is partially blocked. This causes pressure to gradually increase. This pressure damages the optic nerve.
Angle-closure glaucoma
Angle-closure glaucoma, also called closed-angle glaucoma, occurs when the iris bulges forward to narrow or block the drainage angle formed by the cornea and iris. As a result, fluid can not drain out of the eye and pressure increases. Some people have narrow drainage angles, putting them at increased risk of angle-closure glaucoma.
Angle-closure glaucoma may occur suddenly (acute angle-closure glaucoma) or gradually (chronic angle-closure glaucoma). Acute angle-closure glaucoma is a medical emergency.
Normal-tension glaucoma
In normal-tension glaucoma, your optic nerve becomes damaged even though your eye pressure is within the normal range. No one knows the exact reason for this. You may have a sensitive optic nerve, or you may have less blood supply to your optic nerve.
Glaucoma in children
It’s possible, but rare for infants and children to have glaucoma. It may be present from birth or develop in the first few years of life. The optic nerve damage may be caused by drainage blockages or an underlying medical condition.
Pigmentary glaucoma
In pigmentary glaucoma, pigment granules from your iris build up in the drainage channels, slowing or blocking fluid exiting your eye.
Risk factors
Because chronic forms of glaucoma can destroy vision before any signs or symptoms are apparent, be aware of these risk factors:
- Having high eye pressure (intraocular pressure) over 21 mmHg
- Being over age 60
- Being black, Asian or Hispanic
- Having a family history of glaucoma
- Having certain medical conditions, such as diabetes, heart disease, high blood pressure and sickle cell anemia
- Having thin corneas
- Being extremely nearsighted (myopic) or farsighted (hyperopic)
- Having had an eye injury or certain types of eye surgery
- Taking corticosteroid medications, especially eyedrops, for a long time
Prevention
These self-care steps can help you detect glaucoma in its early stages, which is important in preventing vision loss or slowing its progress.
- Get regular eye examinations. Regular comprehensive eye exams can help detect glaucoma in its early stages, before significant damage occurs. As a general rule, it is recommended that you have a comprehensive eye exam every 2 years and every year if you’re older than 65. If you’re at risk of glaucoma, you’ll need more frequent screening.
- Know your family’s eye history. Glaucoma tends to run in families. If you’re at increased risk, you may need more frequent screening.
- Exercise safely. Regular, moderate exercise may help prevent glaucoma by reducing eye pressure.
- Take prescribed eyedrops regularly. Glaucoma eyedrops can significantly reduce the risk that high eye pressure will progress to glaucoma. To be effective, eyedrops prescribed by your optometrist or ophthalmologist (eye specialist) need to be used regularly even if you have no symptoms.
- Wear eye protection. Serious eye injuries can lead to glaucoma. Wear eye protection when using power tools or playing high-speed racket sports in enclosed courts.
Diagnosis
Your optometrist will review your medical history and conduct a comprehensive eye examination. He or she may perform several tests, including:
- Measuring intraocular pressure
- Testing for optic nerve damage with an OCT scan
- Checking for areas of vision loss (visual field test)
- Measuring corneal thickness (pachymetry)
- Inspecting the drainage angle
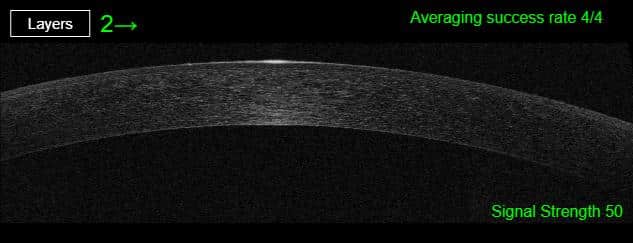
Corneal thickness – pachymetry – Neilson Eyecare
Treatment
The damage caused by glaucoma can’t be reversed. But treatment and regular checkups can help slow or prevent vision loss, especially if you catch the disease in its early stages.
Glaucoma is treated by lowering your eye pressure (intraocular pressure). Depending on your situation, your options may include prescription eyedrops, laser treatment, surgery or a combination of any of these.
Eyedrops
Glaucoma treatment often starts with prescription eyedrops. These can help decrease eye pressure by improving how fluid drains from your eye or by decreasing the amount of fluid your eye makes. Depending on how low your eye pressure needs to be, more than one of the eyedrops may need to be prescribed.
Oral medications
If eyedrops alone don’t bring your eye pressure down to the desired level, your doctor may also prescribe an oral medication.
Surgery and other therapies
Other treatment options include laser therapy and various surgical procedures.
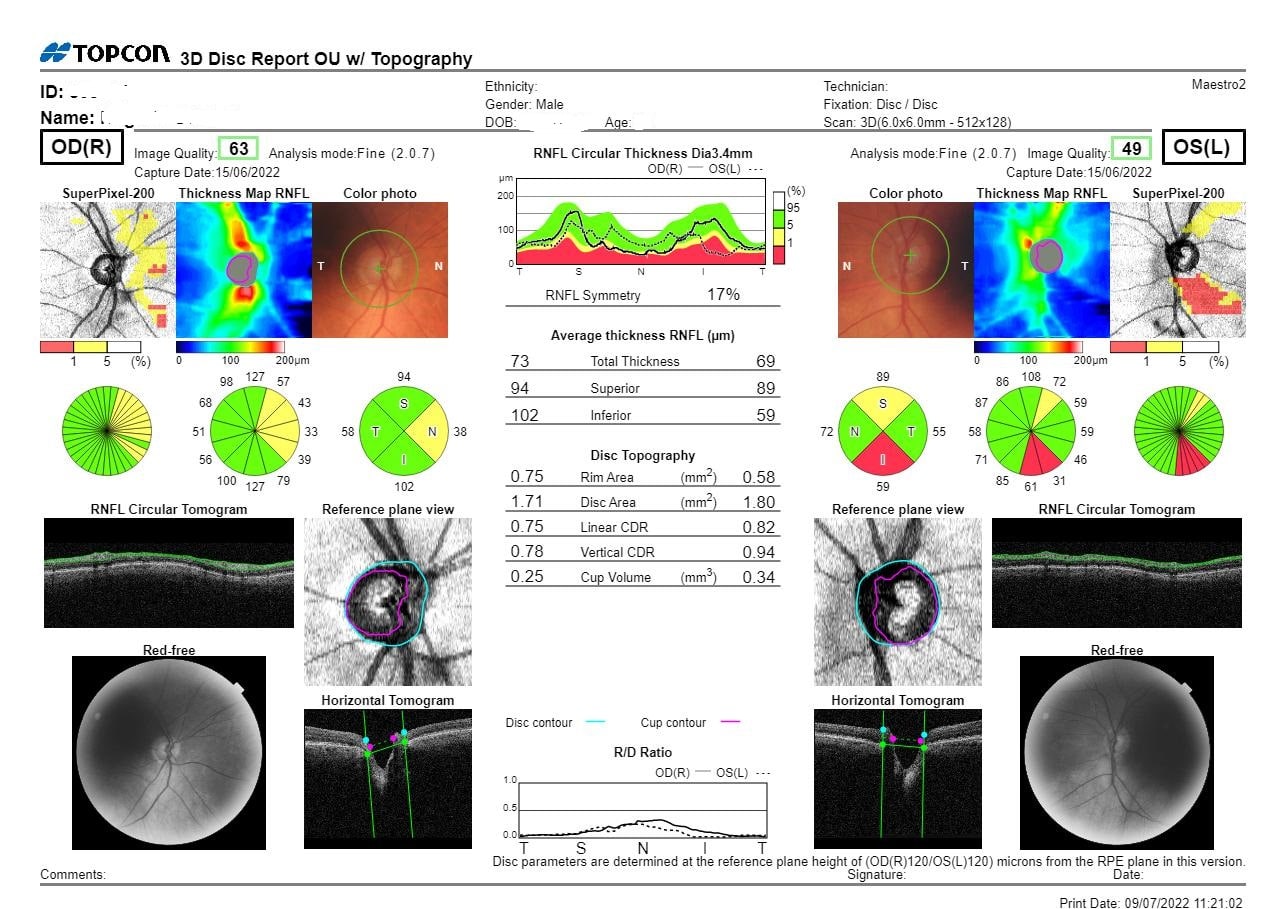
Glaucoma Exam Report – Neilson Eyecare
If you would like more information, free education and support materials to equip you with the skills, knowledge and confidence to take an active role in your glaucoma management plan, please go to the Glaucoma Australia website.
Information sourced from the Mayo Clinic https://www.mayoclinic.org/


